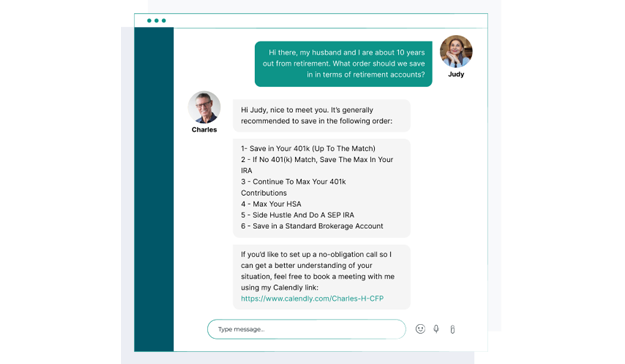
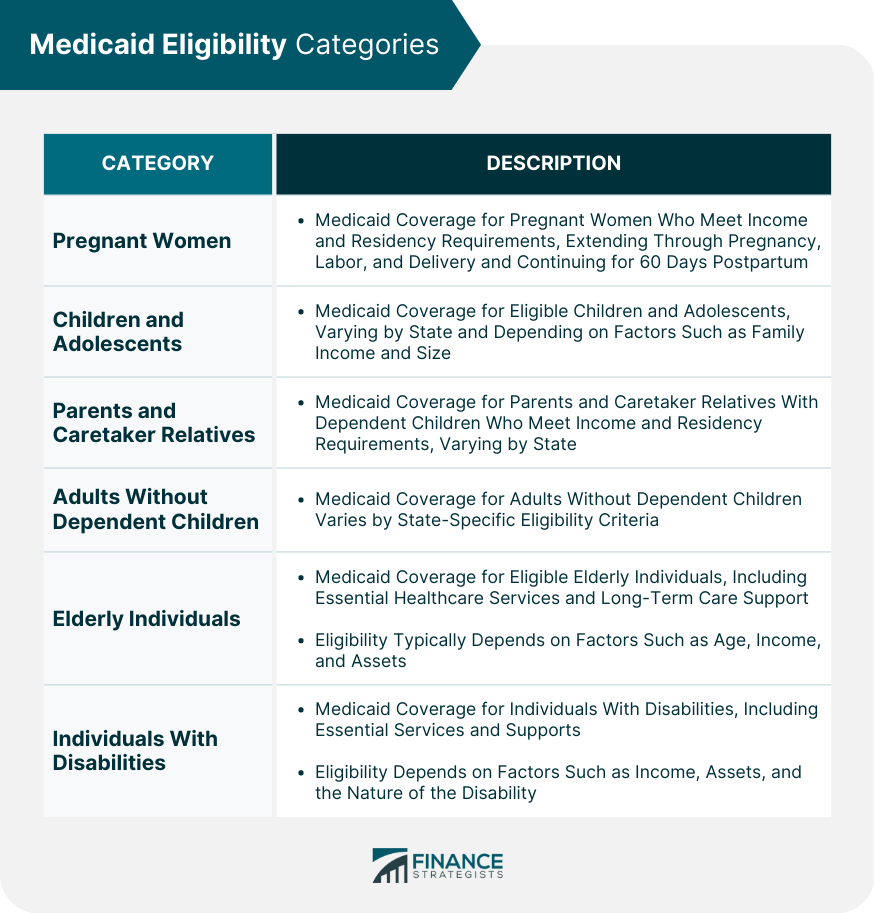
Medicaid is a state and federal partnership that provides health coverage for low-income Americans. This government-funded program aims to improve healthcare access for vulnerable populations. Established in 1965, Medicaid has since undergone several expansions and changes. Today, it serves as a crucial safety net for millions of people, offering a wide range of healthcare services. Eligibility criteria ensure that Medicaid benefits are provided to those in need. By setting specific requirements, the program can prioritize resources for individuals and families facing financial challenges. These criteria vary by state but generally consider factors like income, family size, and certain demographic categories. Understanding eligibility is essential for navigating the application process and accessing benefits. Income is a significant factor in determining Medicaid eligibility. Federal guidelines set minimum income thresholds, which states may adjust to expand coverage further. Most states use the Federal Poverty Level (FPL) as a benchmark to determine income eligibility. The FPL changes annually, so it is essential to stay updated on the latest numbers. To qualify for Medicaid, applicants must be U.S. citizens or have a qualified immigration status. This requirement ensures that the program focuses its resources on the intended population. Non-citizens with certain humanitarian statuses, such as refugees, may also be eligible. It is crucial to understand the specific rules for immigrants to determine eligibility and access healthcare services. Applicants must provide a valid Social Security number (SSN) when applying for Medicaid. The SSN serves as an identification tool and helps determine eligibility. It is important to note that some individuals, such as newborns, may still qualify for Medicaid even without an SSN. In such cases, the application process may involve additional steps. While federal guidelines establish minimum income thresholds, states have the flexibility to set their specific limits. This means that eligibility criteria can differ significantly between states. Some states have expanded their Medicaid programs to cover more people, while others have stricter limits. It is essential to understand the rules in your state when applying for Medicaid. States may extend Medicaid coverage to additional groups beyond federal requirements. These expansions can provide more comprehensive healthcare access to vulnerable populations in the state. For example, some states may offer Medicaid to low-income adults without dependent children. Understanding the additional eligibility groups in your state can help you determine if you qualify for coverage. Medicaid allows states to cover optional eligibility groups, which may include individuals who do not meet the standard criteria. These optional groups can vary significantly between states. Examples of optional groups include medically needy individuals or those receiving home and community-based services. It is crucial to research your state's optional eligibility groups to understand your potential eligibility. Medicaid covers pregnant women who meet income and residency requirements. This coverage aims to ensure proper prenatal and postnatal care, leading to healthier outcomes for both mother and child. Coverage typically extends through pregnancy, labor, and delivery, and continues for 60 days postpartum. In some cases, states may offer additional benefits or extend coverage beyond the standard period. Medicaid provides healthcare coverage for eligible children and adolescents, ensuring access to essential services. This coverage helps address disparities in healthcare access and supports the well-being of younger populations. Children's eligibility depends on factors like family income and size, and the specific rules in each state. In some cases, states may offer additional coverage through the Children's Health Insurance Program (CHIP). Parents and caretaker relatives with dependent children may qualify for Medicaid if they meet income and residency requirements. This coverage aims to support families in need and promote the well-being of both children and caregivers. Eligibility varies by state, and some states have expanded coverage to include a broader range of parents and caretaker relatives. Understanding the specific rules in your state can help determine if you qualify for benefits. Medicaid coverage for adults without dependent children depends on state-specific eligibility criteria. The Affordable Care Act (ACA) enabled states to expand their Medicaid programs to cover this population. Not all states have chosen to expand their Medicaid programs, so eligibility for adults without dependent children can vary. Researching your state's specific rules is essential for understanding your potential eligibility. Medicaid offers coverage for eligible elderly individuals, providing essential healthcare services and long-term care support. This coverage aims to address the unique healthcare needs of older adults, who often face higher healthcare costs. Eligibility for elderly individuals typically depends on factors like age, income, and assets. Some states may also offer additional benefits or support services tailored to the needs of older adults. Medicaid serves as a critical healthcare safety net for individuals with disabilities. Coverage includes essential services and supports to help people with disabilities lead healthy, fulfilling lives. Eligibility for individuals with disabilities depends on factors like income, assets, and the nature of the disability. Some states may also offer additional benefits or support services tailored to the needs of people with disabilities. Most states offer online applications for Medicaid, making the process more convenient and accessible. These platforms typically provide user-friendly interfaces and step-by-step guidance through the application process. Before applying online, gather necessary documents like proof of income, citizenship, and residency. Ensuring you have all required information on hand can help streamline the application process. Paper applications for Medicaid are available for those who prefer a traditional method or face barriers to online access. These applications can be obtained through local social services offices or state Medicaid agencies. When submitting a paper application, ensure you provide accurate and complete information. This can help avoid delays in processing and increase the likelihood of a successful application. In-person assistance is available for individuals who need help navigating the Medicaid application process. This support can be especially valuable for those with limited English proficiency or complex eligibility situations. Local social services offices, community organizations, and healthcare providers may offer in-person assistance. Reach out to these resources to schedule an appointment or find guidance on completing your application. When applying for Medicaid, applicants must provide documentation to verify their eligibility. This may include proof of income, citizenship, residency, and other relevant information. Gather all necessary documents before starting your application to help streamline the process. Providing accurate and complete documentation can increase your chances of a successful application. Medicaid beneficiaries typically receive healthcare services through either managed care or fee-for-service models. Managed care involves enrolling in a health plan, while fee-for-service allows beneficiaries to access providers directly. States have different approaches to these models, and some may offer a combination of both. Understanding the options in your state can help you make informed decisions about your healthcare coverage. Medicaid offers a range of healthcare services, including doctor visits, hospital care, prescription medications, and more. The specific benefits provided depend on your eligibility category and state guidelines. Some states may offer additional benefits or optional services. Familiarize yourself with the benefits available in your state to maximize your healthcare coverage. Access to healthcare providers is an essential component of Medicaid coverage. Beneficiaries must ensure they visit providers that accept Medicaid to receive covered services. Each state maintains a network of participating healthcare providers, including doctors, hospitals, and specialists. It is important to research providers in your area to ensure they accept Medicaid and meet your healthcare needs. Beneficiaries must report any changes in their circumstances that could affect their Medicaid eligibility. Examples of such changes include fluctuations in income, changes in household size, or alterations in residency. Promptly reporting changes helps ensure that beneficiaries maintain accurate and up-to-date coverage. Failure to report changes may result in loss of eligibility or other consequences. Medicaid requires periodic redeterminations to confirm ongoing eligibility for the program. These redeterminations typically occur annually, although the frequency may vary by state. During a redetermination, beneficiaries must provide updated information and documentation to verify their continued eligibility. It is essential to comply with redetermination requirements to maintain coverage. Certain changes in circumstances may lead to a loss of Medicaid eligibility. Examples include increases in income, changes in family size, or gaining access to other healthcare coverage. If you lose Medicaid eligibility, it is crucial to explore alternative healthcare options. Some individuals may qualify for coverage through the Health Insurance Marketplace, employer-sponsored plans, or other state programs. Understanding Medicaid eligibility is essential for navigating the application process, accessing benefits, and maintaining coverage. Familiarizing yourself with the specific rules and requirements in your state can help you make informed decisions about your healthcare. Staying informed about eligibility criteria and available resources can empower individuals and families to access essential healthcare services and improve their overall well-being. Each state has its own Medicaid agency responsible for administering the program, determining eligibility, and providing resources for beneficiaries. These agencies can provide valuable information and assistance throughout the Medicaid process. Reach out to your state's Medicaid agency for guidance on eligibility, application procedures, and available benefits. These agencies can serve as a primary resource for navigating the complexities of the Medicaid program. In addition to state Medicaid agencies, numerous other resources can provide assistance and support. Community organizations, healthcare providers, and advocacy groups can offer guidance and resources for navigating the Medicaid system. Seek out these resources in your community to help you better understand the program and access the healthcare coverage you need. Engaging with these organizations can empower you to take control of your healthcare journey.Overview of Medicaid Eligibility
Federal Requirements for Medicaid Eligibility
Income Thresholds
Citizenship and Immigration Status
Social Security Numbers
State Variations in Eligibility Criteria
State-Specific Income Limits
Additional Eligibility Groups
Optional Eligibility Groups
Eligibility Categories
Pregnant Women
Children and Adolescents
Parents and Caretaker Relatives
Adults Without Dependent Children
Elderly Individuals
Individuals With Disabilities
Application Process for Medicaid
Online Applications
Paper Applications
In-Person Assistance
Required Documentation
Enrollment and Benefits
Managed Care vs. Fee-for-Service
Benefit Packages
Access to Providers
Changes in Eligibility Status
Reporting Changes
Periodic Redeterminations
Loss of Eligibility
Conclusion and Resources
Importance of Understanding Medicaid Eligibility
State Medicaid Agencies
Additional Resources for Assistance
Medicaid Eligibility FAQs
Medicaid eligibility determines who can receive healthcare coverage through the government-funded program. Understanding eligibility criteria is essential for navigating the application process, accessing benefits, and maintaining coverage.
Federal requirements for Medicaid eligibility include income thresholds, citizenship and immigration status, and providing a valid Social Security number (SSN) when applying for Medicaid.
States have the flexibility to set their specific income limits and may extend Medicaid coverage to additional and optional eligibility groups. Understanding the rules in your state is essential when applying for Medicaid.
The specific benefits provided depend on eligibility categories and state guidelines. Beneficiaries must report any changes in their circumstances that could affect their eligibility and comply with periodic redeterminations to maintain coverage.
There are several Medicaid eligibility categories, including pregnant women, children and adolescents, parents and caretaker relatives, adults without dependent children, elderly individuals, and individuals with disabilities.
True Tamplin is a published author, public speaker, CEO of UpDigital, and founder of Finance Strategists.
True is a Certified Educator in Personal Finance (CEPF®), author of The Handy Financial Ratios Guide, a member of the Society for Advancing Business Editing and Writing, contributes to his financial education site, Finance Strategists, and has spoken to various financial communities such as the CFA Institute, as well as university students like his Alma mater, Biola University, where he received a bachelor of science in business and data analytics.
To learn more about True, visit his personal website or view his author profiles on Amazon, Nasdaq and Forbes.