Palliative care is a specialized approach to healthcare that focuses on improving the quality of life for patients and their families facing serious illnesses. Palliative care planning is a critical aspect of this approach, as it involves identifying and addressing the patient’s physical, emotional, and spiritual needs and those of their caregivers. The first step in palliative care planning is to assess the patient's needs and preferences. This involves taking into account their medical condition, symptoms, overall health status, personal values, cultural beliefs, and spiritual needs. It is essential to involve the patient and their family in this process to ensure that their preferences and goals of care are respected. Based on the assessment, the healthcare team can develop a care plan tailored to the patient's needs and preferences. The plan should include specific interventions for managing symptoms such as pain, nausea, and fatigue and addressing emotional and spiritual needs such as anxiety, depression, and existential distress. The care plan should also include goals of care, such as maintaining quality of life, minimizing suffering, and respecting the patient's autonomy. Once the care plan is developed, it is essential to communicate it effectively to the patient and their family. This involves explaining the plan in a clear and understandable manner, answering any questions they may have, and addressing any concerns or fears they may have. It is also important to ensure that the patient and family understand their role in implementing the plan and the role of the healthcare team in providing ongoing support. Once the care plan is communicated, it is time to implement it. This involves ensuring that the patient receives the necessary medical treatments, medications, and supportive care to manage their symptoms and maintain their quality of life. It may also involve providing emotional and spiritual support to the patient and their family, such as counseling or chaplaincy services. Palliative care planning is an ongoing process, and the care plan may need to be adjusted as the patient's needs and preferences change. Regular assessments are necessary to ensure that the care plan remains effective in managing symptoms and meeting the patient's goals of care. The healthcare team should be prepared to make changes to the plan as needed and communicate these changes to the patient and family. One of the palliative care's primary goals is to effectively manage the patient's symptoms. This includes managing physical symptoms such as pain, nausea, and fatigue and psychological symptoms such as anxiety, depression, and delirium. The healthcare team should work closely with the patient and family to identify and address any symptoms affecting the patient's quality of life. Palliative care also involves providing emotional and spiritual support to the patient and their family. This may include counseling, support groups, or chaplaincy services, depending on the patient's needs and preferences. It is essential to recognize the emotional and spiritual aspects of care and provide appropriate support to ensure that the patient and family feel supported and cared for. Advance care planning is an important aspect of palliative care planning. This involves discussing and documenting the patient's preferences for end-of-life care, such as the use of life-sustaining treatments and artificial nutrition and hydration. Advanced care planning helps to ensure that the patient's wishes are respected and that they receive care that aligns with their values and beliefs. It is important to involve the patient and family in advance care planning to understand and document their preferences appropriately. Caring for a seriously ill patient can be emotionally and physically exhausting for caregivers. Palliative care planning should include support for the patient's caregivers, such as respite care, counseling, or education about managing the patient's symptoms. Supporting the caregiver can help to ensure that the patient receives high-quality care and that the caregiver's own well-being is protected. Coordination of care is essential in palliative care planning, particularly when the patient receives care from multiple providers or transitions between care settings. The healthcare team should work closely to ensure that the patient's care is well-coordinated and that all providers are aware of the patient's care goals and preferences. Communication is key in coordinating care, and regular meetings or check-ins can help to ensure that everyone is on the same page. The primary benefit of palliative care planning is improved quality of life for the patient and their family. By addressing the patient's physical, emotional, and spiritual needs, palliative care can help to minimize suffering and enhance well-being. Palliative care planning can also provide support and guidance to the patient's family, helping them to feel more confident and empowered in caring for their loved one. Palliative care planning can also reduce hospitalization and healthcare costs. By effectively managing the patient's symptoms and providing appropriate support and care, palliative care can help to prevent hospital admissions and reduce the need for costly interventions such as emergency department visits or intensive care unit stays. This can result in significant cost savings for patients and healthcare systems. Patients and families who receive palliative care are often more satisfied with their care than those who do not. Palliative care planning can help to ensure that the patient's preferences and goals of care are respected and that the patient and family feel supported and informed throughout the process. This can lead to greater satisfaction with the care they receive and a more positive overall experience. Palliative care planning can also enhance communication and coordination of care between the patient, family, and healthcare providers. By involving the patient and family in the planning process and ensuring that everyone is on the same page regarding the patient's goals of care, the healthcare team can work more effectively together to provide high-quality, patient-centered care. This can lead to better outcomes for the patient and a more positive experience for everyone involved. One of the primary challenges in palliative care planning is the lack of awareness or understanding of palliative care among patients, families, and healthcare providers. Many people associate palliative care with end-of-life care and may be hesitant to engage in palliative care planning if they do not perceive it as relevant to their current health status. Healthcare providers may also lack training or knowledge in palliative care, making identifying and addressing the patient's needs difficult. Effective communication is critical in palliative care planning, but communication barriers can pose a significant challenge. Patients and families may have difficulty expressing their preferences or understanding medical terminology, and healthcare providers may struggle to convey complex information in an understandable manner. Language barriers or cultural differences can further complicate communication and make it challenging to provide high-quality palliative care. Financial barriers can also present challenges in palliative care planning. Patients and families may have limited resources to pay for the necessary care and support services and may not be aware of available resources such as hospice or palliative care benefits. Healthcare providers may also be limited in their ability to provide palliative care services due to financial constraints or lack of reimbursement. Cultural and religious beliefs can also pose challenges in palliative care planning. Patients and families may have different beliefs or values that influence their preferences for care, and healthcare providers may not be familiar with these beliefs or able to accommodate them. Respecting and honoring the patient's cultural and religious background and providing care that aligns with their values and beliefs is essential. Palliative care planning is a critical aspect of palliative care, and it plays a significant role in improving the quality of life for patients and their families facing serious illnesses. The process entails assessing the patient's needs and preferences, developing a tailored care plan, communicating effectively, implementing the plan, and monitoring and adjusting it as needed. There are challenges to palliative care planning, such as lack of awareness, communication barriers, financial constraints, and cultural and religious considerations. On the other hand, the benefits of palliative care planning are significant and include improved quality of life, reduced healthcare costs, increased satisfaction, and enhanced communication and coordination of care. By prioritizing palliative care planning, healthcare providers can help to ensure that patients and families receive the best possible care during a difficult and challenging time. In addition to prioritizing palliative care planning, it is also important for individuals and families to consider estate planning as part of their overall approach to end-of-life care. This involves working with an estate planning lawyer to ensure that one's assets and affairs are in order and that their wishes regarding medical care and distribution of assets are respected. It is important to take action early and not wait until it is too late. Consider seeking the services of an estate planning lawyer to create a comprehensive plan that meets your unique needs and circumstances.What Is Palliative Care Planning?
Process of Palliative Care Planning
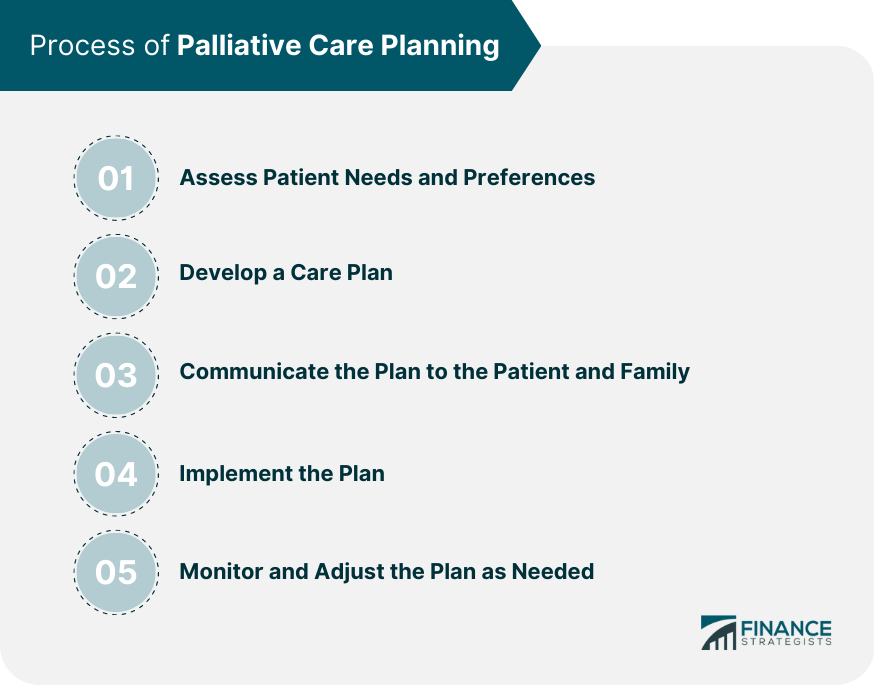
Assessing Patient Needs and Preferences
Developing a Care Plan
Communicating the Plan to the Patient and Family
Implementing the Plan
Monitoring and Adjusting the Plan as Needed
Key Considerations in Palliative Care Planning
Pain and Symptom Management
Emotional and Spiritual Support
Advance Care Planning
Caregiver Support
Coordination of Care
Benefits of Palliative Care Planning
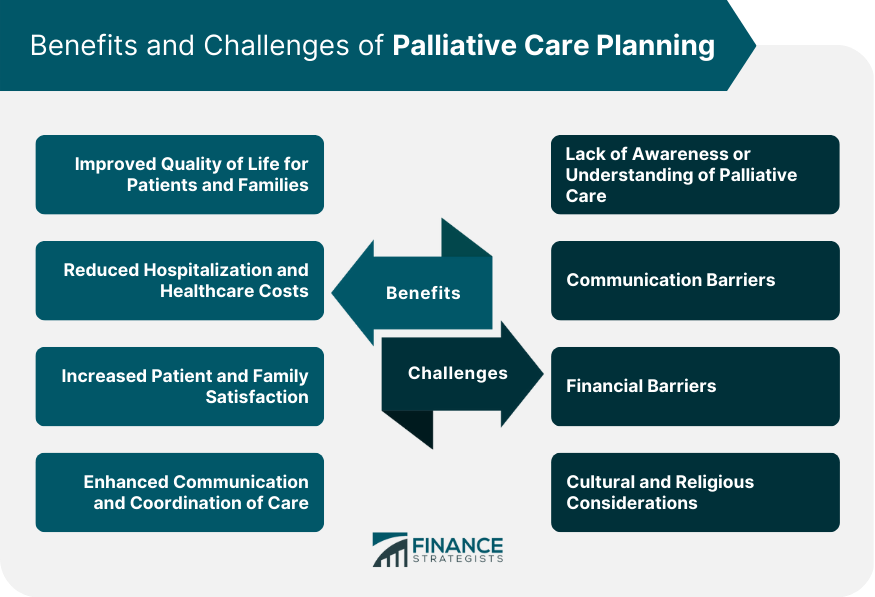
Improved Quality of Life for Patients and Families
Reduced Hospitalization and Healthcare Costs
Increased Patient and Family Satisfaction
Enhanced Communication and Coordination of Care
Challenges in Palliative Care Planning
Lack of Awareness or Understanding of Palliative Care
Communication Barriers
Financial Barriers
Cultural and Religious Considerations
Final Thoughts
Palliative Care Planning FAQs
Palliative care planning is a specialized approach to healthcare that focuses on improving the quality of life for patients and their families facing serious illnesses. It involves assessing the patient's needs and preferences, developing a care plan, communicating the plan to the patient and family, implementing the plan, and monitoring and adjusting it as needed.
Key considerations in palliative care planning include pain and symptom management, emotional and spiritual support, advance care planning, caregiver support, and coordination of care.
Challenges in palliative care planning include lack of awareness or understanding of palliative care, communication barriers, financial barriers, and cultural and religious considerations.
The benefits of palliative care planning include improved quality of life for patients and families, reduced hospitalization and healthcare costs, increased patient and family satisfaction, and enhanced communication and coordination of care.
Estate planning is important in the context of palliative care planning because it involves working with an estate planning lawyer to ensure that one's assets and affairs are in order and that their wishes regarding medical care and distribution of assets are respected. By seeking the services of an estate planning lawyer, individuals, and families can have peace of mind knowing that they have taken steps to protect their loved ones and ensure that their wishes are honored.
True Tamplin is a published author, public speaker, CEO of UpDigital, and founder of Finance Strategists.
True is a Certified Educator in Personal Finance (CEPF®), author of The Handy Financial Ratios Guide, a member of the Society for Advancing Business Editing and Writing, contributes to his financial education site, Finance Strategists, and has spoken to various financial communities such as the CFA Institute, as well as university students like his Alma mater, Biola University, where he received a bachelor of science in business and data analytics.
To learn more about True, visit his personal website or view his author profiles on Amazon, Nasdaq and Forbes.