Medicaid, a crucial joint federal-state program in the U.S., provides essential health coverage to various groups, including low-income individuals, children, pregnant women, the elderly, and people with disabilities. Each state's unique administration of its Medicaid program results in diverse eligibility criteria and benefits, presenting challenges when individuals relocate between states. Such relocations, often driven by career moves, family needs, or lifestyle changes, underscore the importance of uninterrupted healthcare coverage. Successfully navigating these Medicaid transitions is vital. It ensures continuous access to necessary medical care and protects individuals from potential financial difficulties arising from unexpected medical expenses. This continuity is especially critical for those who rely on Medicaid for their healthcare needs. Delving deeper into the nuances of Medicaid's state-specific framework, the discussion turns to the practicalities of how individuals manage their move between states, starting with comprehending the distinct eligibility criteria each state establishes. While Medicaid aims to support individuals with limited financial means, the specifics of this support vary by state. Each state sets its criteria for Medicaid eligibility. Residency criteria, for instance, might look into the duration an individual has lived in the state and their intention to remain there. Financial conditions often delve deep into income, assets, and sometimes even employment status, ensuring that support goes to those who most need it. Transitioning to Medicaid involves more than just a straightforward application. Initially, individuals must notify their current state's Medicaid program about their intent to move. This disenrollment ensures they no longer avail benefits from their former state. Upon reaching the new state, the application process commences anew. This step might seem repetitive, but is essential given the different eligibility criteria and benefits structures. Gathering the right documents and ensuring accuracy can smoothen this phase. Medical histories aren't just files; they are detailed accounts of an individual's health journey. As one transition between states, ensuring medical records follow them is essential. These records guide new healthcare providers in delivering the best care possible. The shift also means finding new healthcare providers that work with Medicaid. Depending on one’s medical needs, this can involve researching specialists, clinics, or hospitals that offer the required services and are within the Medicaid network. The beauty of Medicaid lies in its commitment to ensuring consistent medical care for its beneficiaries. Properly transitioning Medicaid ensures that beneficiaries experience minimal disruptions. This continuous coverage doesn't just offer medical safety—it provides emotional and mental assurance during an otherwise stressful relocation period. Life's unpredictability demands flexibility. Whether for personal growth, family commitments, or chasing dreams, moving states should be free of the added burden of healthcare uncertainties. Moreover, different states may have unique Medicaid benefits, potentially offering better care or more services than the previous state. The fifth benefit of changing Medicaid states is the potential for expanded eligibility in states that adopted Medicaid expansion under the Affordable Care Act (ACA). This expansion allows more low-income adults, particularly those without dependent children, to qualify for Medicaid, enhancing access to healthcare and public health outcomes. Different states mean different Medicaid programs. While some states offer extensive services, others might have a more streamlined approach. There's a potential risk of losing access to specific treatments or services during the transition. This variability demands thorough research and, at times, additional financial planning. Diving into a fresh bureaucratic process can be overwhelming. Each state has its nuances—unique documentation, specific verifications, or even different application portals. Such administrative complexities can lead to delays or miscommunications, potentially causing temporary coverage disruptions. Change, even when beneficial, comes with an adjustment curve. Familiar healthcare providers might no longer be accessible, requiring individuals to build trust with new doctors and medical teams. This phase demands patience and an open-minded approach to healthcare. Understanding the intricacies of Medicaid transitions between states is just the beginning. Implementing practical strategies can greatly facilitate this process. Prior knowledge helps. Before moving, it's invaluable to delve into the Medicaid structures of the prospective state. Such a step aids in setting expectations, preparing necessary documents, and deciding on the move's timing to minimize coverage disruptions. Clear communication bridges many gaps. Current healthcare providers should be informed about the move. Doing so facilitates smoother record transfers. Additionally, engaging with potential healthcare providers in the new state can offer insights into the medical landscape. Timelines shouldn't be an afterthought. Medicaid application processing can vary in duration. By applying promptly upon deciding to move and ensuring all documentation is accurate and ready, individuals can significantly reduce the risk of experiencing coverage gaps. Changing Medicaid from one state to another involves a nuanced journey that reflects the intricacies of the U.S. healthcare system. As individuals relocate, they must traverse through diverse Medicaid programs and cope with state-specific eligibility criteria, application processes, and transition of care. While there are evident benefits, like continuous coverage and adaptability, the process can be riddled with challenges, such as coverage variability, administrative barriers, and adjustment periods. Yet, a smoother transition becomes attainable with informed decisions, detailed research, and proactive communication. The overarching aim remains apparent in the maze of state-specific Medicaid programs: granting uninterrupted access to essential healthcare, regardless of geographical transitions.Medicaid Transition
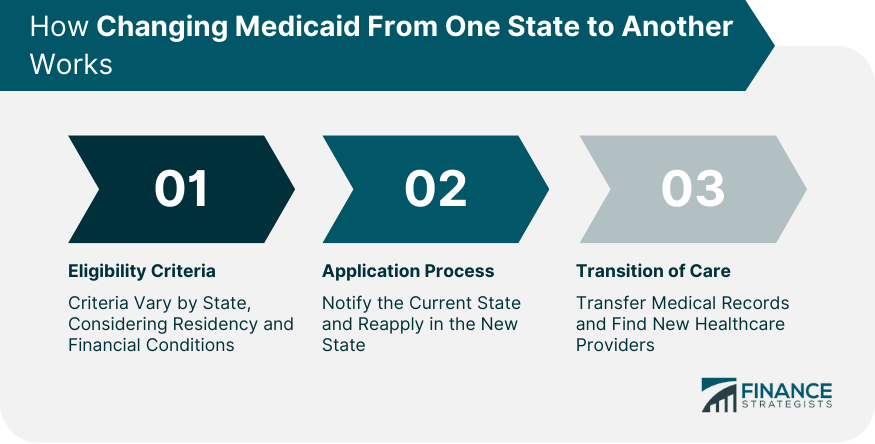
How Changing Medicaid From One State to Another Works
Eligibility Criteria
Application Process
Transition of Care
Benefits of Changing Medicaid From One State to Another
Continuous Coverage
Adaptability to Changing Circumstances
Expanded Eligibility
Drawbacks of Changing Medicaid From One State to Another
Coverage Variability
Administrative Hurdles
Adjustment Period

Practical Tips for a Smooth Medicaid Transition Between States
Research Before Moving
Communication
Timeline and Planning
Conclusion
How to Change Medicaid From One State to Another FAQs
Notify your current state's Medicaid program of your move, disenroll, and then apply afresh in the new form, meeting its specific eligibility criteria.
Some benefits include continuous medical coverage and adaptability to individual needs based on the new state's Medicaid provisions.
Challenges can include coverage variability, administrative hurdles during application, and an adjustment period with new healthcare providers.
Due to varying state-specific criteria and benefits, you must notify and disenroll from your current state's Medicaid and apply in the new state.
Research the new state's Medicaid structure, communicate with your current and potential healthcare providers, and plan the timing of your move to minimize coverage disruptions.
True Tamplin is a published author, public speaker, CEO of UpDigital, and founder of Finance Strategists.
True is a Certified Educator in Personal Finance (CEPF®), author of The Handy Financial Ratios Guide, a member of the Society for Advancing Business Editing and Writing, contributes to his financial education site, Finance Strategists, and has spoken to various financial communities such as the CFA Institute, as well as university students like his Alma mater, Biola University, where he received a bachelor of science in business and data analytics.
To learn more about True, visit his personal website or view his author profiles on Amazon, Nasdaq and Forbes.