Advance directives are legal documents that allow individuals to make decisions about their medical care in advance of becoming incapacitated. These decisions can include what medical interventions they do or do not want, who they want to make medical decisions on their behalf, and what types of treatment they would like to receive in certain situations. Advance directives are designed to ensure that an individual's wishes are honored, even if they are no longer able to communicate them. Advance directives are important for several reasons: First, they help individuals maintain control over their medical care, even if they are unable to make decisions for themselves. This can provide peace of mind and reduce stress for both the individual and their loved ones. Second, advance directives can help prevent family members from having to make difficult medical decisions on behalf of their loved ones. Third, they can help ensure that an individual's values and beliefs are respected and honored in their end-of-life care. These requirements typically include the individual being of sound mind and over the age of 18, the document being signed by the individual and at least two witnesses, and the document being notarized. It is also important to note that advance directives can be updated or revoked at any time, provided the individual is of sound mind and able to communicate their wishes. There are several types of advance directives, including living wills, durable power of attorney for healthcare, do not resuscitate (DNR) orders, and physician orders for life-sustaining treatment (POLST). Each type of advance directive has a specific purpose and addresses different medical interventions. A living will is a legal document that outlines an individual's preferences for medical care in the event they are unable to communicate with them. The purpose of a living will is to provide guidance to healthcare providers and family members in making medical decisions. Common medical interventions addressed in living wills include life support, feeding tubes, hydration, and resuscitation. A living will can be broad or specific in its scope, depending on the individual's preferences. A durable power of attorney for healthcare is a legal document that designates a healthcare proxy, or agent, to make medical decisions on an individual's behalf if they become incapacitated. The purpose of a durable power of attorney for healthcare is to ensure that an individual's wishes for medical care are honored even if they are unable to make decisions for themselves. Appointing a healthcare proxy involves selecting a trusted family member or friend who understands the individual's values and beliefs regarding medical care. A DNR order is a medical order that instructs healthcare providers not to attempt resuscitation if an individual's heart stops or they stop breathing. The purpose of a DNR order is to ensure that an individual's wishes regarding end-of-life care are respected. DNR orders are typically used by individuals with terminal illnesses or those who do not wish to undergo aggressive medical interventions. The implementation of a DNR order may be limited by state laws, hospital policies, or other legal considerations. A POLST is a medical document that outlines an individual's preferences for medical care in an emergency. The purpose of a POLST is to ensure that healthcare providers have clear guidance on an individual's preferences for medical care in a crisis situation. A POLST is different from other advance directives in that it is a medical order that must be signed by a healthcare provider. Key elements of a POLST include preferences for resuscitation, medical interventions, and artificial nutrition and hydration. The first step in creating an advance directive is to assess personal values and beliefs regarding medical care. This involves considering what medical interventions an individual does or does not want in certain situations, such as life support or resuscitation, and how these decisions align with their beliefs and values. This step can be challenging but is crucial to ensure that an individual's preferences are accurately reflected in their advance directive. Once an individual has assessed their personal values and beliefs, it is important to communicate these preferences with family members and healthcare providers. This step can help ensure that everyone is on the same page regarding an individual's preferences for medical care and can prevent confusion or misunderstandings in the future. It is also important to designate a healthcare proxy if an individual chooses to do so and to communicate this choice with the proxy and family members. Advance directives must meet legal requirements to be valid. These requirements may vary depending on the state in which the advance directive is created but often include the individual being of sound mind, the document being properly signed and witnessed, and the document being notarized. It is also important to understand the legal implications of certain medical decisions, such as withholding or withdrawing life support, and to consider working with an attorney to ensure that the advance directive meets all legal requirements. The final step in creating an advance directive is to properly prepare and store the document. The advance directive should be clear and concise, outlining an individual's preferences for medical care in a way that is easy to understand. The document should also be properly stored in a secure location and accessible to family members and healthcare providers in the event it is needed. It is also important to regularly review and update the advance directive as needed, particularly if an individual's preferences or medical situation changes. Regular review of advance directives is important because an individual's preferences for medical care may change over time. Life events, such as a change in health status or the loss of a loved one, may also impact an individual's preferences. Regular review of the advance directive ensures that it accurately reflects an individual's current preferences for medical care and provides guidance to family members and healthcare providers in the event of a medical crisis. Several life events may necessitate changes to an advance directive. For example, a diagnosis of a serious illness may prompt an individual to reconsider their preferences for medical care. A change in family dynamics, such as a divorce or the death of a loved one, may also impact an individual's preferences. It is important to review the advance directive in the event of any significant life changes to ensure that it accurately reflects an individual's current preferences. Once an advance directive has been updated, it is important to communicate these changes to relevant parties. This may include family members, healthcare providers, and the healthcare proxy, if one has been designated. Communicating updates ensures that everyone is aware of an individual's current preferences for medical care and can prevent confusion or misunderstandings in the event of a medical crisis. It is also important to ensure that the updated advance directive is properly stored and accessible to those who may need it. Autonomy refers to an individual's right to make decisions about their own medical care. Advance directives are designed to ensure that an individual's autonomy is respected, even if they are no longer able to make decisions for themselves. However, autonomy can be complicated by issues related to decision-making capacity, or an individual's ability to make decisions for themselves. Healthcare providers must carefully assess an individual's decision-making capacity before following the directives outlined in an advance directive. Advance directives may raise questions related to medical futility, or the idea that certain medical interventions may not be effective or may even be harmful. Healthcare providers may be reluctant to follow advance directives that they believe are medically futile or may conflict with their own values or beliefs. This can raise questions related to physician conscience and the ethical responsibilities of healthcare providers to follow an individual's advance directive, even if they disagree with the decisions outlined in the document. Advance directives may also be subject to legal disputes, particularly if family members or healthcare providers disagree with the decisions outlined in the document. These disputes may be complicated by conflicts of interest, particularly if family members or healthcare providers have their own preferences for medical care that conflict with the individual's advance directive. It is important to ensure that advance directives are properly executed and meet all legal requirements to minimize the risk of legal disputes. Advance directives are an important tool for individuals to plan and communicate their preferences for medical care should they become incapacitated. By creating these documents, individuals can ensure that their wishes are honored and that their loved ones and healthcare providers have a clear understanding of their values and beliefs. Although advance directives can be difficult to confront, planning for end-of-life care is an important part of life, and advance directives can help provide peace of mind for both the individual and their loved ones.What Are Advance Directives?
Importance of Planning for End-Of-Life Care
Legal Status and Requirements of Advance Directives
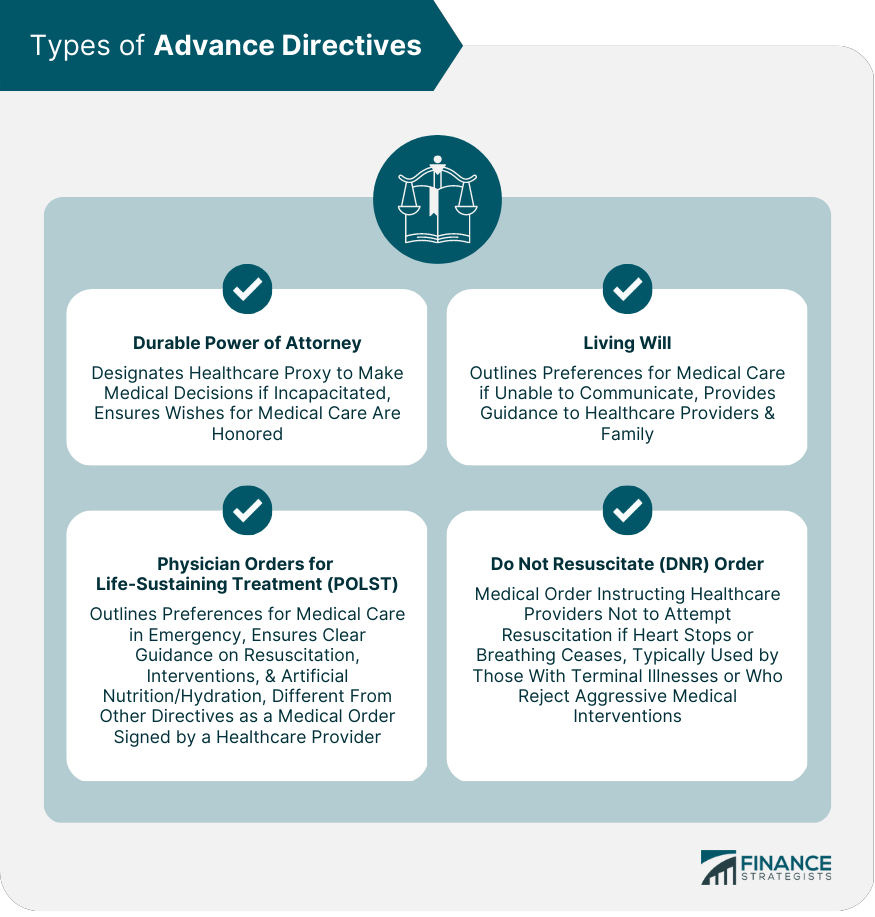
Advance directives are legal documents that vary in their requirements depending on the state in which they are created. However, there are some general requirements that are common across most states. Types of Advance Directives
Living Wills
Durable Power of Attorney for Healthcare
Do Not Resuscitate (DNR) Orders
Physician Orders for Life-Sustaining Treatment (POLST)
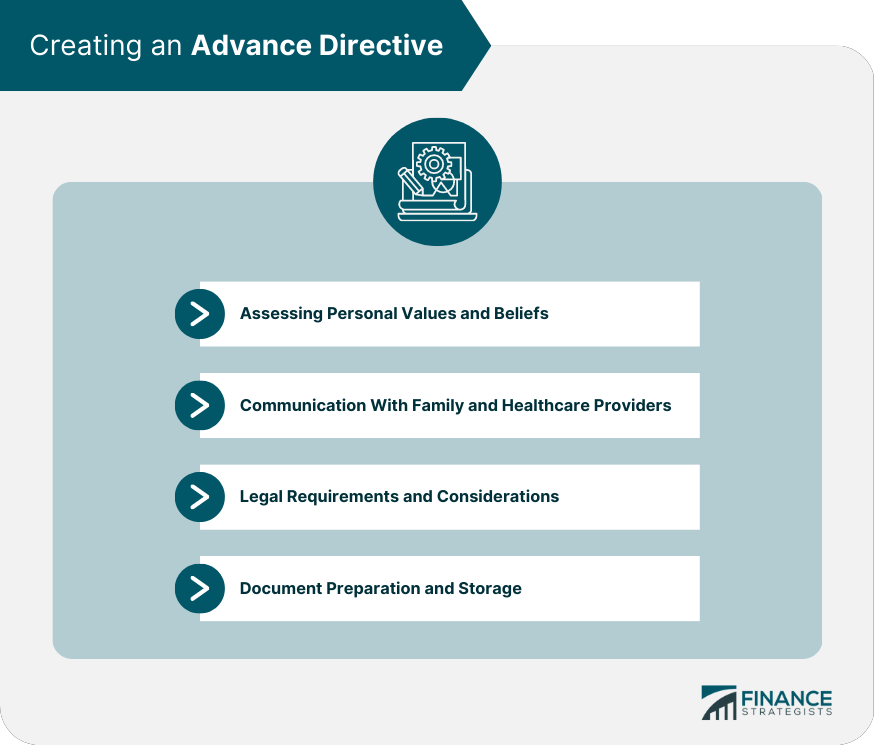
Creating an Advance Directive
Assessing Personal Values and Beliefs
Communication With Family and Healthcare Providers
Legal Requirements and Considerations
Document Preparation and Storage
Updating and Reviewing Advance Directives
Importance of Regular Review
Life Events That May Necessitate Changes
Communicating Updates to Relevant Parties
Ethical and Legal Issues
Autonomy and Decision-Making Capacity
Medical Futility and Physician Conscience
Legal Disputes and Conflicts of Interest
Final Thoughts
Advance Directives FAQs
An advance directive is a legal document that allows you to express your wishes about medical treatment and end-of-life care in case you become unable to communicate your decisions. It can include instructions for life-sustaining treatment, organ donation, and appointment of a healthcare proxy.
You can create an advance directive by consulting with an attorney or using an online template. It's important to have it witnessed and signed in accordance with state laws.
Yes, you can change your advance directive at any time. Simply create a new document, sign and date it, and provide copies to your healthcare proxy and other relevant individuals.
Healthcare providers use advance directives as a guide to make medical decisions on your behalf if you are unable to communicate. They will consult your healthcare proxy and follow the instructions outlined in your advance directive to ensure that your wishes are respected.
The requirements for advance directives can vary depending on the state or country you live in, but generally, they must meet the following criteria: 1) You must be of legal age and have capacity to make decisions, 2) The document must be in writing, 3) It must be signed and dated, 4) It must be witnessed or notarized, and 5) It must be clear and specific about your wishes for medical treatment and end-of-life care. It is important to consult with an attorney or use a reliable online template to ensure that your advance directive meets the legal requirements in your jurisdiction.
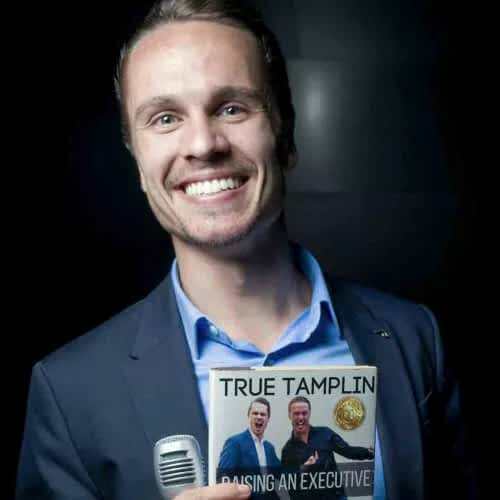
True Tamplin is a published author, public speaker, CEO of UpDigital, and founder of Finance Strategists.
True is a Certified Educator in Personal Finance (CEPF®), author of The Handy Financial Ratios Guide, a member of the Society for Advancing Business Editing and Writing, contributes to his financial education site, Finance Strategists, and has spoken to various financial communities such as the CFA Institute, as well as university students like his Alma mater, Biola University, where he received a bachelor of science in business and data analytics.
To learn more about True, visit his personal website or view his author profiles on Amazon, Nasdaq and Forbes.